Last Updated on January 11, 2023 by pf team
Medical coding continue to be in strong demand as the healthcare industry extends its historic growth. Now may be the perfect time to begin your career as a medical coder.
As the backbone of the healthcare system, medical coding and billing make modern healthcare possible by connecting service providers with insurers to ensure fast processing.
Medical coding classifies healthcare procedures and treatments in a way that both doctors and insurers understand.
Medical billing uses medical codes and standard processes to help ensure that healthcare providers get paid for their services and that claims go smoothly for patients.

In this article :
Reasons to become a medical coder and biller
As the US healthcare industry continues its growth, the future for medical coding and billing looks bright.
Here are some of the top reasons to consider a career in medical coding and billing:
- You’ll be working in the growing healthcare industry. With an aging population, increasing healthcare needs keep demand high for medical billing and coding.
- Demand for medical coding and billing specialists continues to grow. Expect up to 11% growth through 2028 according to Bureau of Labor statistics data. By comparison, BLS job growth projections for all industries is only 5%.
- You don't need to go to medical school. You can train to become a medical coder or biller online and at your own pace. The American Academy of Professional Coders offers online training and certification. In many cases, you can complete your training within 1-2 years.
- Remote jobs for this career are increasingly popular. Because you're working with data, medical coding and billing work is a good fit for remote work. Often, you can enjoy a flexible schedule and work from the comfort of home.
- You’ll find plenty of opportunities to move up the ladder. As you gain experience or earn new certifications, you'll find more opportunities for advancement. You can also expect higher average annual earnings as you gain experience.
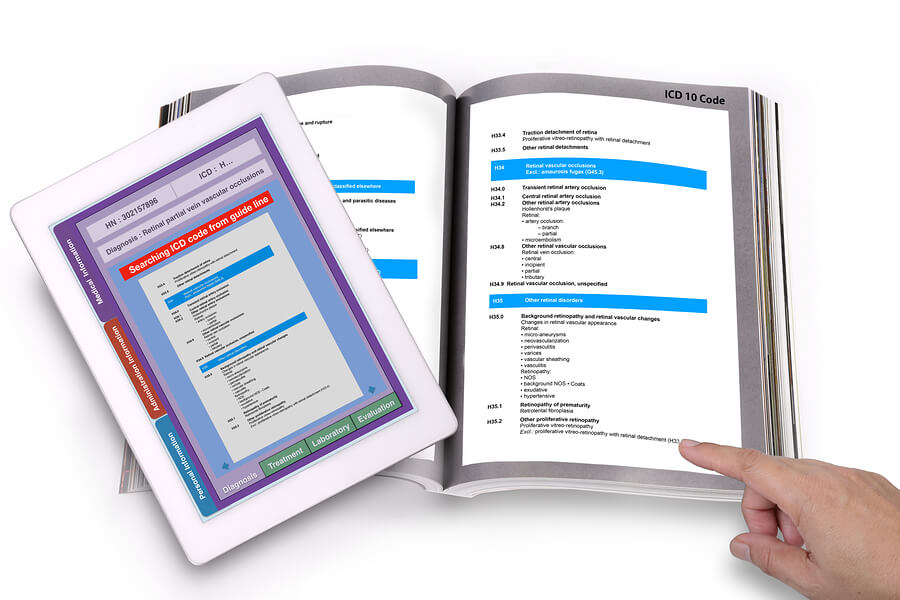
What is medical coding?

When working in medical coding, you’ll convert medical services and procedures to the following groups of codes:
- Diagnostic codes: Medical treatments begin with an exam and diagnosis. As a medical coder, you’ll translate the descriptions of diseases, illnesses, and injuries into their medical classifications.
- Procedure codes: The various procedures used in healthcare also have medical codes. Procedure codes can refer to the actual procedures performed but can also refer to medical equipment or medications given to the patient.
- Pharmaceutical codes: Each type of medication has a code as well. However, medical pharmaceutical codes can refer to a specific type of medicine or to an active ingredient.
- Topographical codes: In medical coding, topographical codes (or topography codes) refer to a specific area of the body. These codes are helpful to both doctors and insurers because they specifically identify the area affected by illness or injury.
What is medical billing?
Medical codes use a universal coding system to classify illnesses or injuries as well as treatments. These codes can be used to track and understand illnesses but they're also an essential part of medical billing.
In most cases, healthcare is provided as part of a 3-party system which includes the doctor and patient, but which also includes the insurer.
Often, the insurer pays the lion's share of healthcare expenses and medical billing must follow a specific format.
Medical billing uses medical codes to create invoices that can be tracked and paid by the insurer. It's also common for patients to pay a portion of their medical expenses.
- Front-end medical billing: Front-end billing refers to the portion of the bill for which the patient is responsible. Examples include copayments, deductibles, or procedures not covered by the insurer.
- Back-end medical billing: Back-end billing refers to Insurance claims and amounts that should be paid by the insurer. Standardized forms are used depending on the type of treatment and coverage. For example, a medical biller might use form CMS-1450 to submit a claim under Medicare Part A. However, a CMS-1500 might be used to submit a claim under Medicare Part B.
What does a medical coder and biller do?
In some job environments, medical coders are distinct from medical billers. In other cases, daily tasks are split between the two roles. Depending on your role and certifications, you may spend part of your day coding and another part of your day billing.
Your daily duties can include the following tasks:
- Analyze patient’s records, including diagnosis and treatment
- Convert diagnosis and treatment descriptions to standardized medical codes
- Use standardized medical codes to invoice patients and submit claims to insurers
- Work closely with doctors and assistants to ensure the accuracy of coding
- Submit claims to insurers and follow up on payments
- Submit invoices to be paid by patients
- Interact with patients regarding insurance and billing matters
Skills needed for a medical coding and billing career
Your training can give you the knowledge you’ll need to work in medical coding and billing. However, you’ll also need some key traits and basic skills.
- You’ll benefit from basic computer knowledge. Much of your work centers on using a computer or a dedicated terminal and specialized software.
- Discretion and integrity are also key. Because you'll be working with personal information for patients, discretion is a must. In fact, HIPAA protections that ensure medical privacy also govern the way medical billing must be submitted in claims.
- You’ll also need thoroughness. Accuracy is key when coding and billing. Even small errors or omissions can create delays or denied claims.
- Above all, you’ll need analytical thinking. Context can play a big role in medical billing and there may be multiple ways to bill a procedure. Your ability to analyze all the factors is key.
- Knowledge of medical science and terminology is essential. A big part of your job is to translate medical jargon and records into standardized codes. You won’t need to perform any medical procedures yourself, but you'll need to understand the diagnosis and the treatment to properly code these items.
Medical coding salary

Income opportunities look bright for medical coders and billers. AAPC offers average income data dating back to 2006, showing steady growth.
For 2018, the average annual income for medical coders with any type of certification through AAPC was nearly $55,000. For medical coders with any type of specialty certification through AAPC, average annual earnings exceed $60,000.
Expect your earnings power to increase as you add additional certifications. For example, the average annual income for medical coders with 3 or more AAPC credentials reached nearly $70,000 in 2018.
AAPC also reports that on-site workers earn slightly less on average than their remote counterparts. Remote workers earn as much as $4,000 per year more on average, although the number of credentials held may also play a role.
Medical coding training
You’ll find courses for medical coding and billing from several sources including local and online options. Some choose to attend a local college, but you can often earn your certification online.
Choosing an online course may be more affordable and allows you to train at your own pace.
One popular choice for online medical coding training is AAPC. The American Academy of Professional Coders has trained and certified hundreds of thousands of healthcare industry workers.
With nearly 200,000 members worldwide and 28 certifications available, AAPC provides a solid starting point when you’re ready to give a new direction to your career.
AAPC offers nearly a dozen popular and highly regarded certifications for medical coding and billing.
Medical coding and billing certifications
CPC
Still the most common medical coding certification available through AAPC, a CPC certification demonstrates your broad skill as a Certified Professional Coder. AAPC estimates that coders with the CPC designation can earn up to $20,000 more than those without the certification.
COC
As a Certified Outpatient Coder, you’ll boost your average annual earnings. Nationwide, medical coding and billing professionals with a COC certification earn nearly $60,000.
Earning your COC certification opens the door for work at outpatient surgical centers and other medical facilities with specialized outpatient billing needs.
CIC
For inpatient specialization, consider the Certified Inpatient Coder certification offered by AAPC.
Expect your work to center around hospitals and other inpatient facilities that require specialized billing knowledge, including Medicare Severity Diagnosis Related Groups.
CRC
Earning an average of nearly $10,000 more per year than the average medical coding professional, a Certified Risk Adjustment Coder is a highly sought-after designation.
With this specialized certification, you demonstrate your knowledge of risk adjustment models, including Health and Human Services risk adjustment.
Specialty
Experienced coders recognize the value of specialty certifications. While also earning a CPC certification can be helpful, AAPC offers 18 unique specialized certifications that stand on their own.
Choose from pediatrics, ophthalmology, family practice, and more.
CPB
To document your expertise in medical billing, consider earning a Certified Professional Biller certification.
You’ll submit claims and resolve denied claims but your CPB certification assures employers that you’re highly trained, which minimizes the risk of error-related claim denials.
On average, CPB certified professionals earn more than $52,000 per year.
CPMA
Cash flow is the lifeblood of any business and as a Certified Professional Medical Auditor, your role is to find the revenue-cycle bottlenecks related to medical coding and billing.
Your CPMA certification validates your knowledge of guidelines and processes, making you a professional in high demand. Average earnings for CPMA-certified professionals approaches $67,000 annually.
CDEO
With a Certified Documentation Expert Outpatient (CDEO) certification, you’ll open the door to higher income.
On average, CDEO-certified professionals earn over $69,000. Think of a CDEO professional as an expert consultant in medical coding and billing.
You’ll work directly with providers to examine documentation and improve standards going forward.
CPCO
With new laws and guidelines changing the coding and billing landscape, a watchful eye on compliance is invaluable.
As a Certified Professional Compliance Officer, you’ve shown your expertise in compliance with ever-changing rules and requirements.
You’ll become the go-to person for compliance reviews, and even staff training. With one of the highest-paying certifications, CPCO-certified professionals earn an average of more than $74,000 per year.
CPPM
Providing a pathway to a management role, earning your certification as a Certified Physician Practice Manager offers a bump in salary as well as a more expansive job role.
You’ll gain detailed knowledge of all the major medical coding and billing processes in physician offices.
Because your role focuses on management, you’ll also master other skills, such as marketing and human resource matters.
On average, annual incomes for CPPM-certified professionals come close to $70,000.
Medical coding and billing jobs at flexjobs.com

With the right credentials, you’ll find plenty of opportunities to work in medical coding.
Flexjobs.com can be a great place to start your search, especially if you prefer flexible hours or remote work. AAPC found that remote workers often earn more.
For medical coding, we found nearly 1,600 job listings on FlexJobs. Most offered full-time work and nearly 2/3 offered 100% remote work or remote work as an option.
We found similar results for medical billing jobs. Although we found fewer job listings, more than half offered 100% remote work or the option of working remotely.
Top 5 medical billing and coding employers for flexible work
By choosing the right employer, you can gain valuable experience and add consistency to your resume.
Fortunately, some of the biggest names in healthcare also offer both on-site work and remote work. Again, FlexJobs provides the perfect place to start your search.
UnitedHealth Group
Expect competitive benefits and a selection of part-time, full-time, and flexible schedule jobs.
Up to 90% of the jobs posted by UnitedHealth Group on FlexJobs.com were for remote-work positions. Up to 90% of the healthcare giant’s job listings were full-time as well.
Aetna
One hundred percent of Aetna’s job listings on FlexJobs have been for remote work positions. All of Aetna’s positions were also employee positions, which means you may qualify for benefits not available to freelancers.
Expect this employer to lean heavily toward full-time work.
Humana
Like Aetna, Humana favors employees over freelancers. The company also focuses its listings on full-time remote work jobs.
Expect industry-leading benefits like tuition assistance and more. For flexibility combined with the perks of working with a Fortune 500 company, take a closer look at Humana.
Anthem
Although headquartered in Indianapolis, Anthem employs workers from all over the country. The company serves over 10% of the US population and operates several regional Blue Cross and Blue Shield companies.
Several specialty companies under the Anthem banner create additional employment opportunities.
Parallon
Perhaps the most focused of the larger healthcare employers on FlexJobs, Parallon offers revenue cycle management services for hospitals and similar healthcare facilities.
Revenue cycles refer to cash flow and that means opportunity for coders and billers. Parallon’s listings focus on full-time and remote work, with a strong preference for employee hires as opposed to using freelancers.
Medical coding and billing FAQs

Is medical coding in demand in the USA?
Medical coding and billing remain in high demand in the US, with expected growth of over 10% during the next several years.
Job openings can be competitive, and experience is a plus when searching for employment. It's often best to seek related employment while you're in school to earn your medical coding certification.
How long does it take to become a certified medical coder?
The amount of time required to earn your certification depends on the level or types of certification you choose.
For example, you can earn a basic certification for physician-based coding in less than 1 year. Certification for facility-based coding might require 1 year of training or longer.
How do I become a medical coder?
For some medical coding schools, you'll need a high school diploma or equivalent to qualify. Background checks are also common. Your next step is to enroll in a program to earn your certification.
In most cases, you can earn your certification in 18 to 24 months, although some certifications require less time.
Which Coding Certification is best?
The CPC certification is most common certification and demonstrates general knowledge in the field. However, your earning opportunities increase with other certifications.
For example, by earning either a CDEO or CPPM certification, average annual salary can increase by nearly $15,000 per year when compared to a base CPC certification.
Is medical coding hard?
Like most things, medical coding becomes easier as you gain exposure and experience. At first, the terminology can seem confusing.
While there are literally thousands of medical codes you can work with as a medical coder, specialized software helps you to find the correct code assignment.
Your ability to work with powerful tools and databases also helps make your work easier.
Can you take the CPC exam online?
The CPC exam is a proctored exam held at approved locations throughout the US. While the exam itself can't be completed online, you can complete your training prior to the exam online and at your own pace.
How much does it cost to take the medical coding exam?
To take the CPC exam through AAPC, you can pay as little as $399. However, this price includes a membership discount. You'll need to be a member to earn your CPC certification through AAPC, so becoming a member is often a good investment.
Financing is also available, which can help to make earning your certification more affordable.
Can anyone take the CPC exam?
The CPC exam measures your detailed knowledge of medical coding. The exam consists of 150 questions in 24 subject areas and takes nearly 6 hours to complete.
CPC Certification through AAPC also requires on-the-job experience or an apprenticeship. It’s best to invest in a course designed to help you earn your CPC certification before signing up for the CPC exam.
What medical coding certification pays the most?
According to data from AAPC, Medical coders with a CPC-I (Certified professional coding instructor) or a CPCO (Certified professional compliance officer) certification earned the highest average salaries in 2018.
In both cases, the average annual salaries for 2018 came in at over $70,000. By comparison, the average annual salary for someone earning any AAPC Credential was about $54,500 in 2018.
Where do medical coders work?
Medical coders work in nearly every area of healthcare. Hospitals, for example, might employ dozens of medical coders. Specialized offices often employ several, whereas smaller physician offices may only keep one or two medical coders or billers on staff.
Third-party medical billing businesses are also becoming more common, with many of these employers offering remote work.
The final word on medical coding
With the right credentials, a career in medical coding and billing can be financially rewarding. Fortunately, with a tiered system for credentialing, you can work while you earn your next certification.
Even a base CPC certification puts you in demand in a career group that’s expected to grow for years to come.